Understanding Physiological Factors in Abdominal Adipose Tissue Accumulation
An educational resource exploring the science behind fat distribution patterns and metabolic factors influencing abdominal adiposity.
Subcutaneous vs Visceral Adipose Tissue
Anatomical and Functional Differences
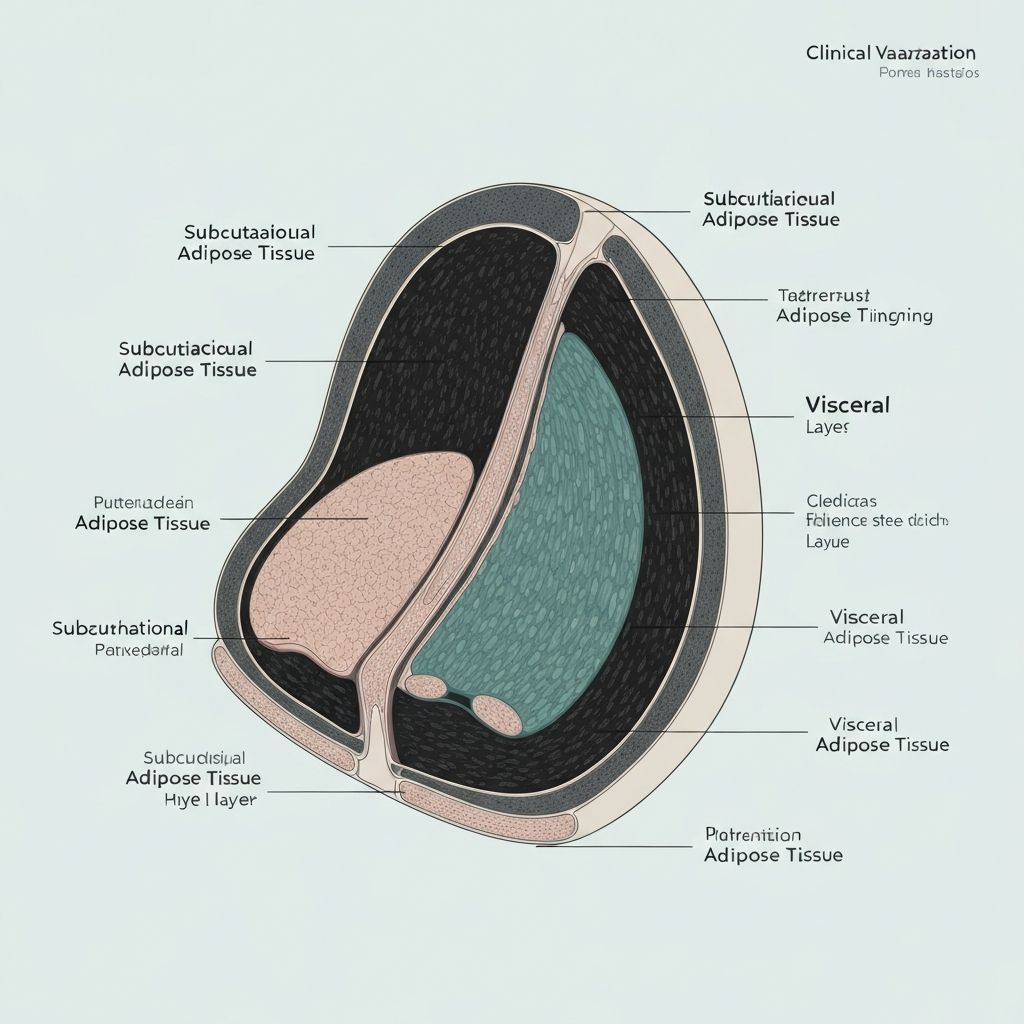
Abdominal adiposity manifests in two distinct compartments, each with unique physiological characteristics and metabolic implications. Subcutaneous adipose tissue lies beneath the skin and above the abdominal muscles, while visceral adipose tissue resides within the peritoneal cavity, surrounding internal organs.
These compartments differ significantly in their cellular composition, metabolic activity, and endocrine function. Visceral fat exhibits greater metabolic turnover and produces higher levels of inflammatory cytokines and adipokines compared to subcutaneous reserves.
Cortisol and Chronic Stress Influence
Glucocorticoid Effects on Central Fat
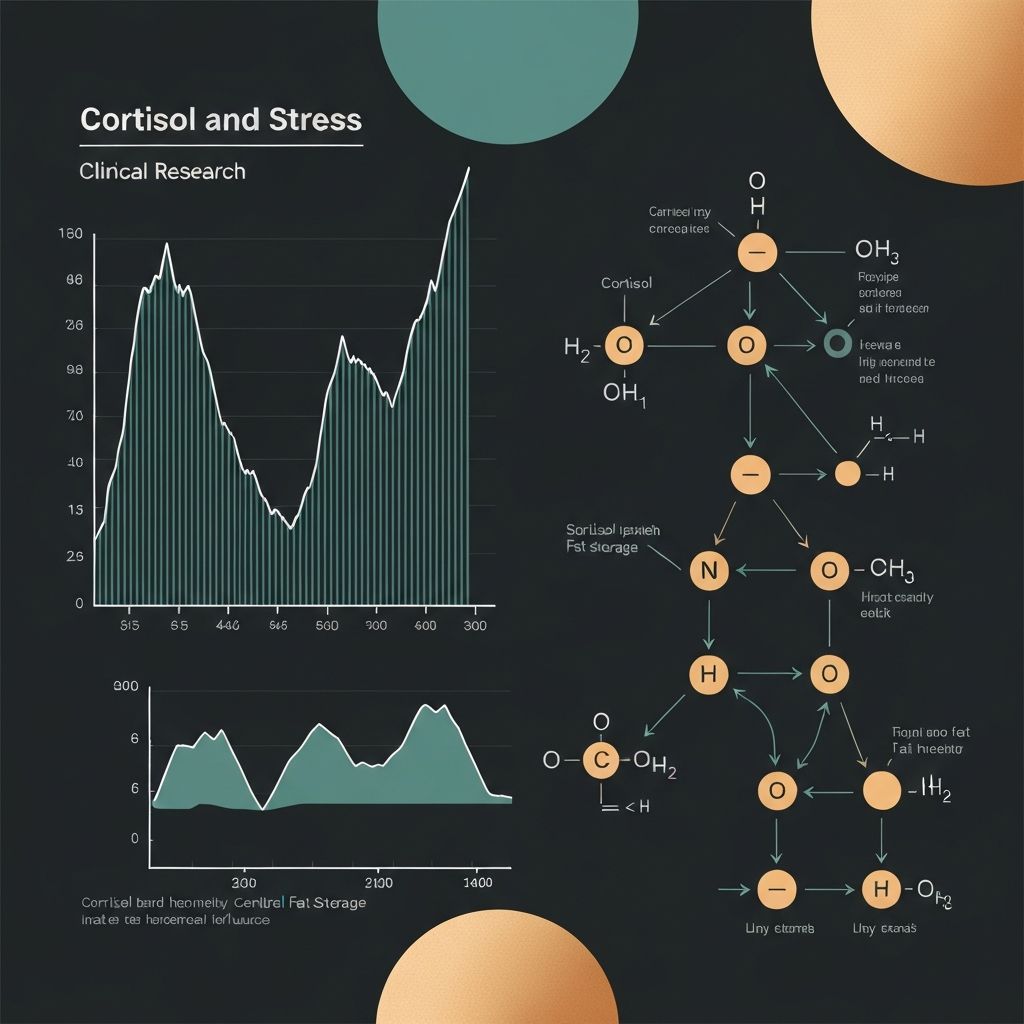
Chronic activation of the hypothalamic-pituitary-adrenal (HPA) axis and sustained glucocorticoid elevation demonstrate preferential effects on central fat accumulation. Cortisol, the primary human glucocorticoid, influences adipocyte differentiation, lipogenic enzyme expression, and substrate partitioning toward visceral compartments.
Research on cortisol-adiposity relationships documents that prolonged psychosocial stress and dysregulated diurnal cortisol patterns associate with increased waist circumference and visceral fat deposition, particularly in midlife populations.
The mechanisms involve enhanced lipoprotein lipase activity in visceral adipose tissue, increased free fatty acid uptake, and altered glucose homeostasis promoting central storage patterns.
Insulin Sensitivity and Hyperinsulinaemia
Role in Abdominal Storage Patterns
Chronic hyperinsulinaemia and reduced insulin sensitivity demonstrate strong associations with central fat accumulation and visceral adiposity. Elevated fasting insulin concentrations reflect both pancreatic compensation for insulin resistance and direct effects on lipid metabolism and substrate availability.
Insulin resistance promotes preferential storage in visceral compartments through several mechanisms: enhanced lipogenic gene expression, suppression of hepatic fatty acid oxidation, and increased glucose uptake into abdominal fat depots.
Observational cohort studies and intervention trials document that improved insulin sensitivity, achieved through various lifestyle patterns, associates with reductions in central adiposity and waist circumference.
Sex-Specific Hormonal Patterns
Androgens and Estrogens in Fat Distribution
Sexual dimorphism in abdominal fat distribution reflects the influence of sex hormones on adipocyte development, metabolic fate, and regional lipid storage. Androgens in biological males suppress subcutaneous fat accumulation while promoting visceral adiposity, whereas estrogens in biological females direct fat storage toward subcutaneous depots and gluteal-femoral regions.
Changes in sex hormone concentrations during midlife transitions (perimenopause and andropause) correlate with shifts toward greater central fat accumulation in both sexes. Postmenopausal women demonstrate accelerated visceral fat gain compared to premenopausal counterparts despite stable body weight.
Testosterone administration in hypogonadal males associates with reductions in central adiposity, while estrogen therapy in perimenopausal women influences fat distribution patterns independently of weight change.
Low-Grade Inflammation and Adipokine Imbalance
Visceral adipose tissue exhibits elevated inflammatory activity compared to subcutaneous reserves, producing elevated concentrations of pro-inflammatory cytokines including interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). This chronic inflammatory state contributes to systemic metabolic dysfunction and may promote further central fat deposition.
Adipokines—secreted proteins from adipose tissue—demonstrate imbalanced production in visceral obesity. Reduced adiponectin secretion and elevated leptin resistance characterize visceral adiposity, affecting systemic insulin sensitivity and energy homeostasis. The inflammatory milieu of visceral fat promotes lipid infiltration into liver and muscle, exacerbating metabolic dysfunction.
Sleep Duration and Quality Effects
Epidemiological observations consistently document that short sleep duration and poor sleep quality associate with increased central adiposity and waist circumference independent of total caloric intake and physical activity patterns. Sleep deprivation impairs glucose homeostasis, enhances sympathetic nervous system tone, and alters hormone concentrations promoting central storage.
Mechanistically, insufficient sleep elevates ghrelin (appetite hormone) while suppressing leptin signaling, favoring lipid accumulation. Circadian rhythm disruption—common in shift work and modern schedules—directly impairs metabolic regulation and may preferentially promote visceral fat deposition. Recovery studies demonstrate that improved sleep architecture associates with favorable changes in central adiposity measurements.
Observational Associations with Waist Trends
Large prospective cohort studies document correlations between dietary composition patterns and waist circumference trends. Observational data suggest associations between high added sugar and refined carbohydrate consumption and increased central adiposity, whereas diets emphasizing whole grains, legumes, vegetables, and minimally processed foods correlate with lower waist circumference despite similar caloric intake.
These associations reflect both metabolic differences in nutrient handling and indirect effects on energy balance and physical activity engagement. Important to note: observational associations document correlation, not causation, and individual responses vary substantially based on genetic, behavioral, and contextual factors.
Longitudinal Cohort Insights
Prospective studies tracking fat distribution across midlife transitions reveal consistent patterns of central adiposity accumulation independent of total body weight changes. Women transitioning through perimenopause document 5–15% increases in visceral fat compartment size over 3–5 year periods, with acceleration during the final menstrual transition years.
Men demonstrate comparable midlife visceral fat accumulation during ages 40–60, associated with declining testosterone and metabolic rate reductions. These longitudinal observations underscore that fat distribution patterns shift substantially across the lifespan, reflecting cumulative effects of hormonal, metabolic, and behavioral factors operating over years and decades.
Explore Detailed Fat Distribution Topics
Learn more about specific physiological mechanisms influencing abdominal adiposity.
Subcutaneous vs Visceral Differentiation
Detailed examination of anatomical compartments and their distinct metabolic properties.
Cortisol and Central Fat Storage
Comprehensive exploration of stress hormone effects on abdominal adiposity patterns.
Insulin and Metabolic Partitioning
In-depth analysis of insulin's role in directing nutrients toward central adiposity.
Sex Hormones and Fat Distribution
Detailed study of androgen and estrogen influences on regional fat patterning.
Inflammation and Adipokine Dysregulation
Comprehensive review of inflammatory mechanisms in visceral adiposity.
Sleep and Circadian Regulation
Detailed exploration of sleep's influence on fat distribution and metabolic fate.
Frequently Asked Questions
Disclaimer: Educational Content
The materials on this site are purely educational and informational in nature. This content does not constitute nutritional, medical, or body composition guidance. Individual fat distribution patterns vary substantially based on genetics, age, sex, and numerous environmental factors. No specific outcomes should be expected from reading this information. For personalized health or medical concerns, consult qualified healthcare professionals. This resource explains physiological phenomena; it does not provide individualized recommendations or promise outcomes.
Continue Exploring Adipose Tissue Regulation Topics
Discover more in-depth physiological and research context through our comprehensive articles.
Explore All Articles